Are we all chimera?
Our cells don’t all contain the same genome: some of them come from other individuals. Known as microchimerism, this phenomenon questions our vision of immunity and of human biological identity: we are all (micro)chimera!
Investigation by Lise Barnéoud - Published on
A new discipline in biology
It’s a science that is currently emerging, a new field of research that calls into question much of our knowledge. We used to think that we were made up of cells with an identical genome, all from our first zygote, a fusion between the ovum and the spermatozoa. In reality, we are all hosts of cells from other individuals. The phenomenon is known by scientists as microchimerism, in reference to the mythological Greek monster made up of several different species. But here this term refers to organisms made up of cells with different genetic origins. Thus, unlike the common equation "one individual = one genome", several human genomes cohabit inside our bodies.
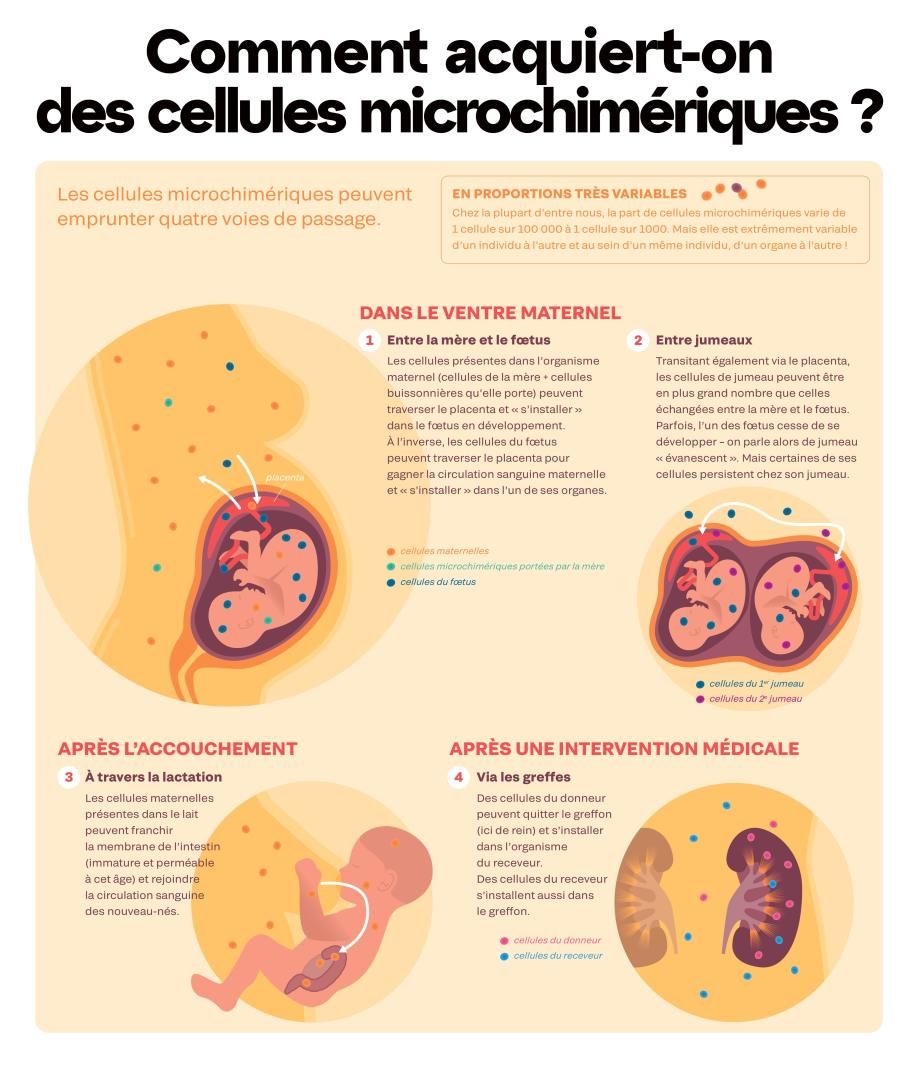
For a century now, researchers have suspected that our cells travelled on both sides of the placenta. In 1893 a German researcher identified cells from foetuses in the lungs of women who had died during pregnancy or childbirth. In 1953 it was discovered that twins exchange cells in utero. And in the 1960s, publications wrote about cells from the mother discovered in newborns. At the time we imagined that the immune system would reject these "foreign" cells, otherwise a pathological process would be triggered. Thirty years later, biologists showed that this was not the case: these cells remain and most of the time are well tolerated. These "travelling cells" are the subject of growing interest: despite being few in number, they influence our physiology, our immunity and our neurone development. They thus open up new opportunities in medicine.
The womb as the epicentre of exchange
At the end of 2023, researchers were able to view the passing of the mother’s cells through the placenta’s various membranes, to the foetus’s bloodstream. Through this same mechanism, twins can also exchange cells. This is known as "twin chimerism". These cells from a twin are sometimes found in such large quantities that they make up entire organs! In rare cases they are found inside reproductive organs, which can scramble genetic lineage.


The sum of our parts
In 2021 a French study dropped a small bombshell: cells from maternal grandmothers were found in the blood of 18% of newborns tested (5 out of 28 newborns). Thus pregnant women can transfer not just their own cells to their foetus, but also other cells such as those from their own mother.
But that’s not all! Since these cellular journeys take place in all directions, during their reproductive lives, women accumulate cells from all the embryos they have carried: Even in cases of miscarriage or abortion, cells invade the mother’s body.
These cells can cross back through the placenta and enter a developing foetus. In this way we can also inherit cells from foetuses who developed before us in our mother’s womb.
Another possible source of microchimerism, but one which is not yet demonstrated, is the mother’s elder siblings, or twin, living or vanishing (foetus of a twin that did not develop). Years later, these cells could cross back through the placenta during a pregnancy. "There are probably other sources of microchimerism that we don’t yet know about", explains Lee Nelson, who has devoted his career to studying the phenomenon at the Fred Hutchinson Cancer Center in Seattle. The proof is that in 2005 a study revealed that over 60% of stillborn female foetuses and 80% of girls under the age of 2 possessed male microchimeric cells in their liver. Most of them without any male twin or elder brother reported...

Our children and our mothers in our brains!
In 2022, a study conducted in mice showed that cells from the mother can cross the blood-brain barrier and influence the foetus’s neurone development. In 2012, a prior study involving 54 deceased women showed that 63% of the women had male cells in their brains! The study did not reveal where the cells came from, nor whether they were neurones or other types of cells in our brains. Since then, studies in animals suggest that in the weeks following childbirth, foetal cells can indeed transform into neurones in the mother’s brain.
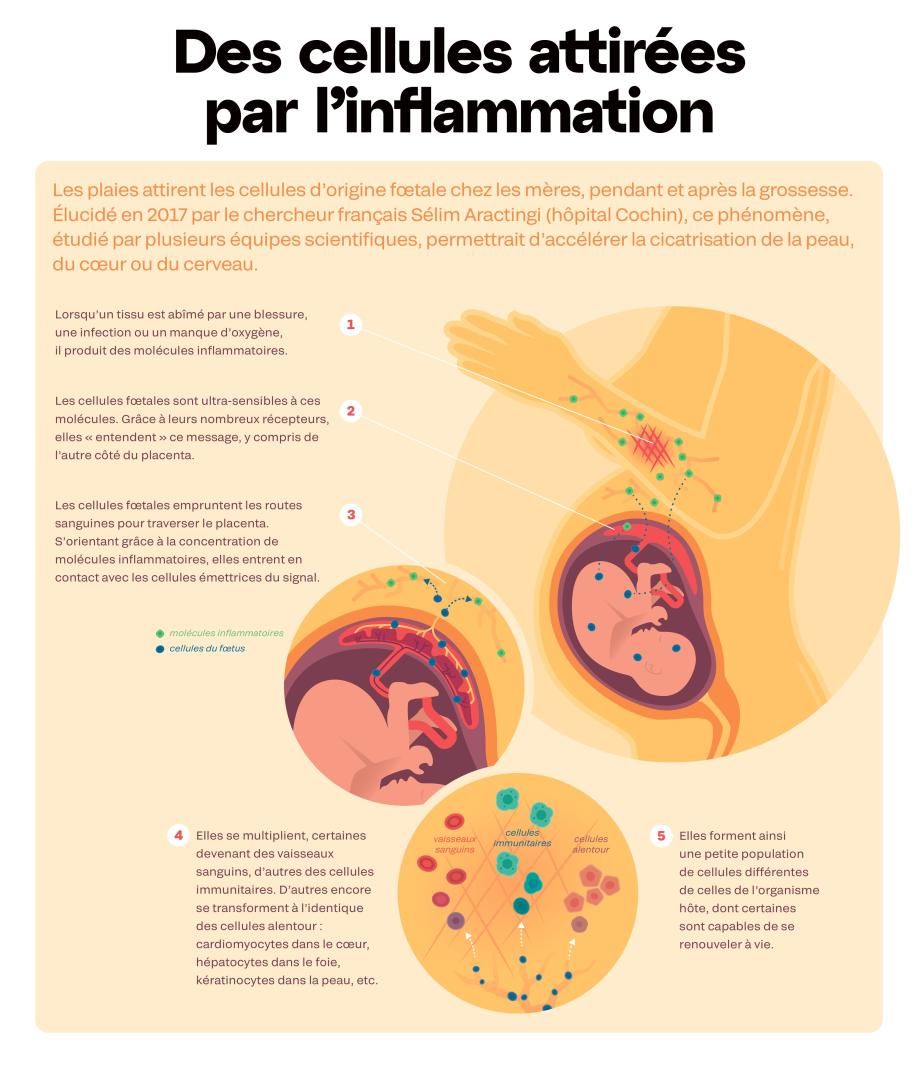
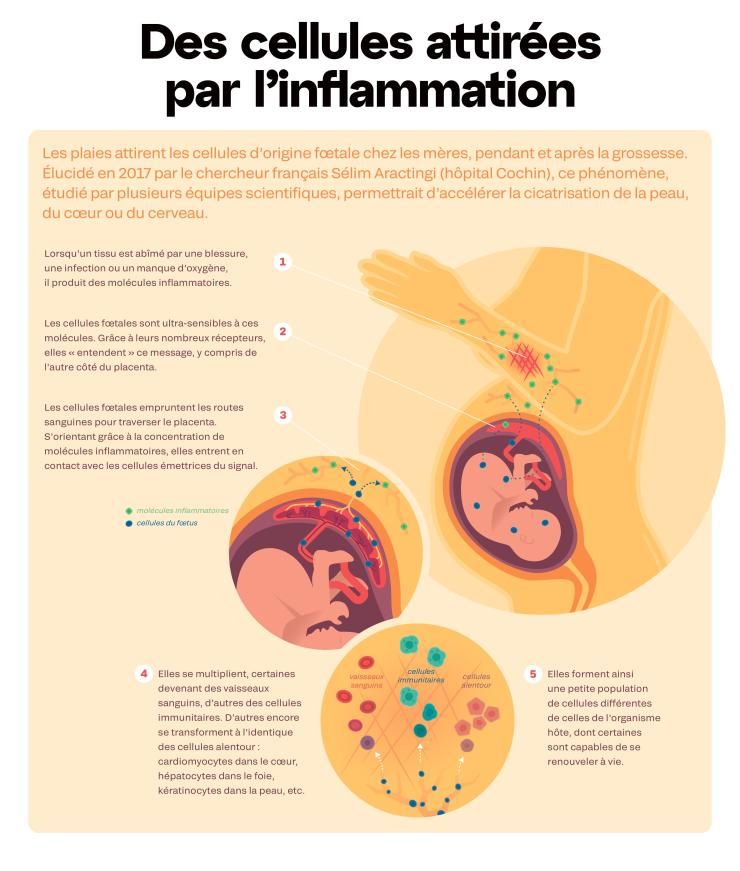
The many advantages of microchimerism
Until the 2000s, research focused above all on identifying rare microchimeric cells. Today the aim is to understand their role. Far from being passive travellers, they play a part in the physiological activities of tissues. Like the stem cells present in all of us, they are undifferentiated and able to generate all types of cells in the human body. If they settle in a heart, they become cardiomyocytes, able to beat alongside other cells. In the skin they become skin cells, etc. They are therefore likely to repair tissues by replacing damaged cells. This makes for a promising outlook in regenerative medicine.
The mother’s cells passed on to the foetus apparently have two types of beneficial effects for the future babies. They promote immunity and "create optimal conditions for healthy brain functioning later in life", explains Petra Arck, Professor of Foetal-Maternal Medicine in Hamburg.
Microchimerism could also represent an advantage for reproduction. "These cells seem to act as negotiators to facilitate the insulation of this semi-foreign body, i.e. the baby to be born, in the mother’s body", explains the US biologist Any Boddy. Furthermore, by settling in the mother’s bloodstream that supplies the placenta, these cells enlarge their diameter and increase the flow of nutrients and oxygen to the foetus. Finally, they promote lactation and block their mother’s ovulation, which is a good way to preserve the mother’s exclusive attention for as long as possible, by delaying the arrival of a younger sibling!
The mother’s cells to the rescue
In the pancreas of a young boy who died of diabetes, researchers discovered several dozen cells carrying two X sex chromosomes (red dots). These are female cells. An analysis of genetic markers showed that these cells came from the boy’s mother. And that’s not all: the researchers discovered that these cells were able to produce insulin. So they could supply this essential hormone to the child, while his own pancreas had become unable to produce it. Not enough, however, to keep him alive.

The dark side of microchimerism
"These cells are neither intrinsically good nor intrinsically bad", declares Dr. J. Lee Nelson, a US specialist in microchimerism. For most of us, cells from different genetic origins coexist with no problems.
But sometimes things don’t go so well. "Depending on the quantity of cells that settle and their genetic characteristics, the balance may be upset" suggests Nathalie Lambert, biologist at Inserm and specialist in microchimerism. And so the blood of individuals suffering from auto-immune diseases more frequently contains microchimeric cells, and in greater quantity. Furthermore, women are more affected in general by auto-immune diseases and the symptoms most frequently appear after pregnancies, after the influx of foetal cells. Hence the hypothesis of a causal link, not yet demonstrated: microchimeric cells may be targeted by the host’s immune system which identifies them as foreign bodies. In this case, it is no longer a question of "auto"-immune diseases, since our immune system attacks not its own cells, but the foreign "travelling" cells.
These microchimeric cells could also settle inside a tumor and take part in the production of new blood vessels that contribute to the spread of cancer. This would explain why the prognosis for certain cancers (skin, breast) is worse if they occur during pregnancy or just after delivery, when the concentration of circulating foetal cells is highest.
Microchimerism with macro-consequences
In 2024, the team of Nathalie Lambert, a biologist at Inserm, showed that we can inherit genetic predispositions carried by our traveling cells. When a mouse "recovers" microchimeric cells (regardless of provenance) carrying a gene that predisposes to rheumatoid arthritis, specific proteins for the disease are identified in its blood, antibodies involved in destruction of the joint. "We don’t yet know if the quantities measured can trigger the disease", explains Nathalie Lambert."But it is proof that even in small quantities these cells can produce proteins that can be detected in the blood."
A new look at immunity
At the turn of the millennium, we discovered the presence of billions of microbial cells in our bodies, known as our microbiote. We therefore have as many human cells as bacterial cells! With microchimerism we are now becoming aware that our human condition is not made up exclusively of our own cells: some of them come from other individuals. "The self means being made by others, being made from others", explains immunologist Edgardo Carosella and philosopher Thomas Pradeu in their book "L’Identité, la part de l’autre." These discoveries have revolutionized our understanding of the body and of human identity. "We are not the products of a pure and homogeneous self-built self", emphasizes Thomas Pradeu.
Microchimerism, like the microbiote, calls into question our traditional vision of immunity as an intolerant system, which identifies the non-self in order to destroy it. The omnipresence of foreign cells, on the contrary, shows that it is a far more tolerant system, in which "differences become precisely what keeps the world together", suggests the Italian philosopher Roberto Esposito.
And taking these reflections further, some thinkers propose adopting an ecological outlook on the individual: from now on considering it as a diverse entity, a collection of cells. Ecologists demonstrated it a long time ago: the more species an ecosystem has, the greater its ability to overcome the vicissitudes of life. Could it be that we are also more efficient and more resilient since we are chimeric?
Interwoven, therefore supportive?
By interweaving our cells, could microchimerism strengthen family cooperation? This is the hypothesis put forward by researchers specialized in the Callithrix, a species in which every family member helps to raise the young. Some of these small monkeys have very large quantities of travelling cells (that come in particular from their many twins), present in the hair, saliva and skin. This helps relatives to recognize scents. The result, observed empirically by researchers, is that newborns with chimeric cells in these tissues are more often carried by their father than those that don’t have them.